What happens to a person’s blood sugar when they are under stress due to pain, and must take a narcotic pain reliever such as oxycodone? In this article, we will explore what happens to a person with diabetes who is taking long term pain medication. We will look at whether it raises or lowers blood glucose.
We will look at how taking oxycodone affects blood glucose levels, activity levels and appetite, and how that could influence the self-management of diabetes. We will look at ways that you can maintain blood glucose in target ranges while taking a narcotic pain reliever such as oxycodone.
John’s story
As John relayed to me during a phone conversation, he is taking a combination of oxycodone plus acetaminophen for severe pain in his legs related to poor circulation and neuropathy because of his Type 1 diabetes. He has had severe sleep disruption, and was getting no relief on nonsteroidal anti-inflammatory agents.
He has been taking oxycodone now for about three months, and has seen a need to increase the basal rate on his insulin pump in order to stay in target range with his blood glucose. He found that once the stress of the pain was gone, his numbers have stayed in range.
I suggest reading the following:
Contents
What is oxycodone?
Oxycodone is a narcotic pain reliever that is used to relieve moderate to severe pain. It is in the class of drugs called “opiate analgesics,” and can be found in combination with other nonsteroidal anti-inflammatory medications such as aspirin, acetaminophen, or ibuprofen. Oxycodone can also be found in combination with aspirin and acetaminophen. Each of these components can also have side effects in addition to the oxycodone.
Brand names of combination medications include Nortab, Vicodin, and Lortab and Percocet.
Precautions for oxycodone products containing aspirin, acetaminophen, or ibuprofen:
- NSAIDs like ibuprofen can harm kidneys and cause stomach upset.
- High dose acetaminophen or Tylenol can harm the liver
- Aspirin may be contraindicated in some patients because of bleeding due to stomach ulcers or other factors, and in people whose asthma is worsened by aspirin
- Make sure you do not take more acetomenophin, ibuprofen, or aspirin on top of the medication in the combination medicine. For example, you wouldn’t take 2 Tylenol along with your oxycodone/acetaminophen combination, due to it already contains Tylenol or acetaminophen
Oxycodone works in your brain to alter pain pathways and the sensation or feeling of pain. For those needing pain relief 24 hours per day, there is Oxycontin. Oxycontin is a timed-release version of oxycodone. These narcotics come with a high propensity for abuse, and many who have taken the drug for 3 months or more still end up taking it up to 5 years after the initial use.
Oxycodone comes in pill form as fast acting or extended release, and in liquid form.
Side effects and adverse reactions with oxycodone
Let’s look at some of the side effects and adverse events associated with oxycodone:
- Confusion
- Agitation
- Nervousness
- Hallucinations
- Trouble sleeping
- Anxiousness
- Depression
- Suicidal thoughts or behaviors
- Slow heart beat
- Fast heart beat
- Palpitations
- Low blood pressure
- High blood pressure
- Orthostatic hypotension (when blood pressure drops drastically upon standing)
- Impaired thinking
- Slow reaction time
- Indigestion
- Stomach pain or swelling
- Diarrhea
- Dry mouth
- Nausea
- Vomiting
- Pancreatitis
- Intestinal blockage or ileus
Serious, life threatening side effects and adverse events:
- Allergic reaction
- Swelling of face, lips, throat
- Difficulty breathing
- Hives
- Tremors
- Convulsions
- Swelling in the brain
- Electrolyte imbalance
- Ringing in ears, and loss of hearing
- Low blood sugar
- High blood sugar
- Increased protein in the urine
- Increased intracranial pressure
- Liver disease
Other things to avoid while taking oxycodone
Avoid alcohol
Alcohol and opioids don’t mix. Mixing the two can cause increased sleepiness, dizziness, confusion, and blurred vision. It also increases the likelihood of an adverse event, such as shallow breathing, or even death due to respiratory failure. Alcohol if taken without food, can cause a marked low blood glucose up to 48 hours following consumption.
Avoid drinking grapefruit juice
Grapefruit juice has been known to interfere with the body’s metabolism of oxycodone, which in turn increases undesirable side effects of the medication.
Do not drive or operate heavy machinery
The best practice is to never drive or operate heavy machinery while taking oxycodone.
It is illegal to drive while under the influence of narcotic medication such as oxycodone if it does indeed impair your driving ability. Some people have an increased tolerance, and may not feel dizzy or impaired, at which point they may think that it is ok for them to drive or operate heavy machinery while on oxycodone.
If you do feel that you are not impaired while taking oxycodone, and you do drive, you will want to carry your prescription with you. A police officer that pulls you over could ask for you to take a saliva test for narcotics. This can be a medical defense, as long as you are not driving while impaired. Remember that if you are swerving or driving recklessly, that you are breaking the law.1
History and present crisis of oxycodone addiction in the US
The FDA (Food and Drug Administration) approved oxycodone for use in 1976. Since then, the abuse of oxycodone and oxycontin extended release has become a national epidemic in the US. Law enforcement officers and EMS personnel now carry Naloxone kits, which contain Narcan, a drug that can reverse the effects of narcotics and save lives during an overdose.
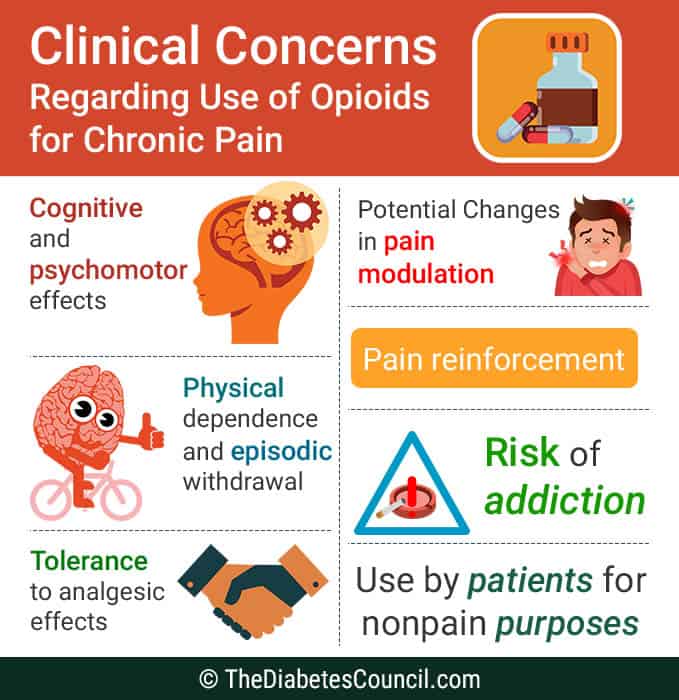
For this reason, doctors and healthcare providers are hesitant to prescribe narcotics for pain relief, especially long term. Narcotics can suppress respirations, especially in a person who has asthma or other breathing issues.
In the US alone, there have been more than 100,000 deaths attributed to oxycodone and other prescribed opioid narcotics since the late 1990’s when drug policies were loosened, allowing physicians to prescribe the medication more readily, according to the 2014 statement from the AAN (the American Academy of Neurology.2
How can oxycodone and pain effect diabetes?
In the description on the package insert for aspirin/oxycodone combination medication, the literature reads:
“Diabetes patients - Aspirin/oxycodone may affect your blood sugar. Check blood sugar levels closely. Ask your doctor before you change the dose of your diabetes medicine.”3
Oxycodone and high blood glucose
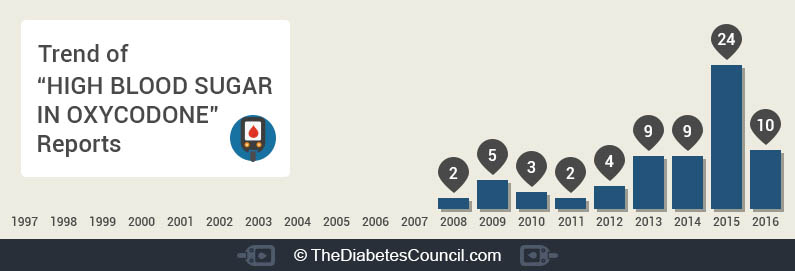
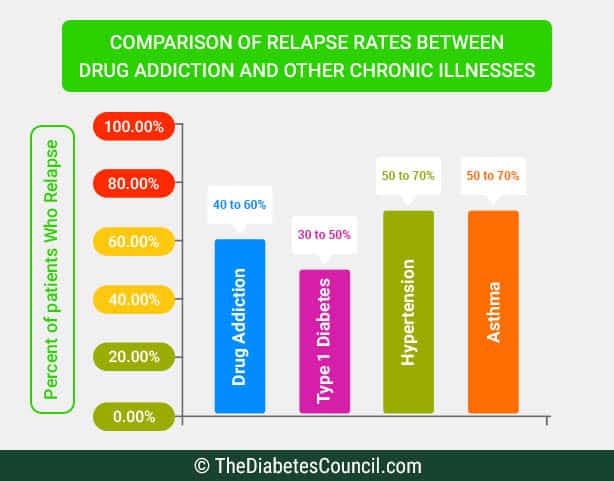
On ehealthnow, 23,272 people reported that they take oxycodone and also have diabetes. Of those, only 68 people reported that they have high blood glucose while taking oxycodone. Seeing that it is such a small number, it does seem possible to get safe, effective pain relief with oxycodone, especially when related to hyperglycemia. The graph below represents the people who reported hyperglycemia on ehealthnow:4
Opioids and low blood glucose
Opioids don’t fare so well related to low blood glucose. In one study of a milder opioid, Tramadol, people taking Tramadol had a 52 percent higher risk of developing a low blood glucose that landed them in the hospital compared with those who took codeine for pain.
This study was done at the University of Montreal, and was published in JAMA Internal Medicine. One important finding Is that Tramadol reduced blood sugar to dangerously low levels in persons with diabetes, but also in persons without diabetes. The hypoglycemia mainly occurred within the first 30 days of use of the milder opioid.5
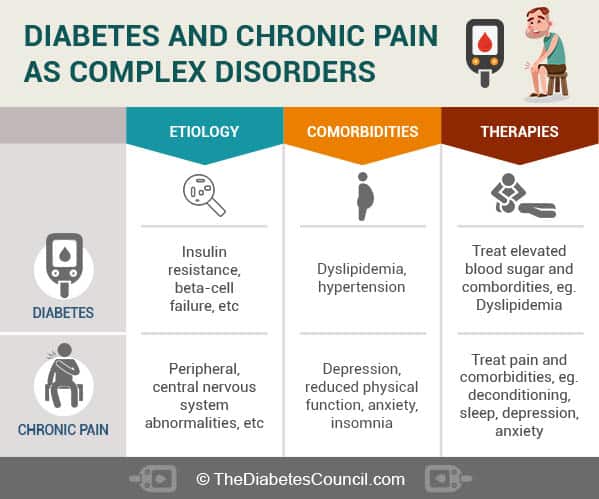
Pain increases stress in the body, causing a release of stress hormones including cortisol, which can help to account for high blood sugars somewhat. Combine that with a decreased activity level, oxycodone tablets to make you sleepy, and a propensity to consume more carbohydrates related to a “narcotic high”, and there you have it- a recipe for diabetes self-management destruction.
Opioid narcotics such as oxycodone kill pain, and they also kill or dull your perception of it. When this happens, decreased perception of what to do to self-manage your diabetes also occurs. People with diabetes who take opioids for pain can often neglect self-care, even missing insulin injections or forgetting to eat regular meals and snacks with insulin already in their system.
This apathy toward care can put a person with diabetes who takes opioids for pain at an increased risk for a low blood glucose, a high blood glucose, or even diabetic ketoacidosis.
Can I take oxycodone safely if I have diabetes?
In one study, controlled release oxycodone was found to be effective and safe to manage pain related to diabetic neuropathy, and was found to increase the patient’s quality of life.6
However, in my experience, there are many diabetics that are having trouble to control their diabetes when on narcotic pain relievers. They tend to gain weight, be less active, and express difficulty with maintaining the level of diabetes control that they had prior to being placed on an opioid pain reliever.
My personal experience as a Certified Diabetes Educator
This makes sense to me. As a person born with congenital hip dysplasia, as the hip joints deteriorated before the total hip replacements were done, taking oxycodone caused significant weight gain, an inability to really “care” whether I ate right or got exercise, and a sort of apathy that I don’t recall ever having to deal with before being placed on opioids.
Apathy is not so good for diabetes self-management. Diabetes is a 24/7 disease, so to effectively self-manage diabetes, you must be on top of it. If you are sleeping more, and moving around less, eating more, and even forgetting medications due to a “euphoric high,” it’s easy to see how that could sabotage the very best self-managers.
Combine that with addiction, and the inability to effectively wean off narcotics without severe withdrawal symptoms, and you have another problem on top of your diabetes that serves to make your diabetes worse. Weight gained from inactivity can cause blood glucose levels and A1C levels to increase. People who once had control over their diabetes find that their diabetes is getting the upper hand.
All this combined is indeed a big problem for the person with diabetes, especially considering that 4 out of 10 persons with the disease have some form of related pain, either from diabetes (such as neuropathy), or from comorbid conditions such as arthritis.
Does oxycodone cause a “sweet tooth?”
It was found in a study published in the Journal of Opioid Management that opioid narcotics such as oxycodone cause a change in taste with a preference for sweetened foods. Persons with diabetes taking opioids should have an awareness of these issues, and be extra diligent to combat the apathy that causes them to miss injections, meals, or other treatments.
Does oxycodone affect insulin absorption?
Oxycodone stimulates the secretion of both insulin and glucagon, while suppressing other hormones in the body. It is possible that long term use of oxycodone increased insulin resistance with related weight gain and inactivity.
Line up your support team if you take oxycodone and have diabetes
Having a good support person or system of people to help to remind you to take medications, check blood sugars, and eat regularly can help the person with diabetes avoid opioid related hypoglycemia, hyperglycemia, or diabetic ketoacidosis.
Ask your healthcare provider about alternative treatments for pain
Physical therapy, massage therapy, TENS units, relaxation, and meditation could be some things that would benefit you to decrease your pain instead of oxycodone.
In my opinion, if the above measures are instituted, it is then possible to have safe and effective use of opioid narcotics medications such as oxycodone if you have diabetes. To make sure, I decided to ask a few of my patients with diabetes how their self-management was going while they were taking opioids. The response somewhat surprised me, as many of my patients are experiencing major self-management issues due to being on opioids.
Request the first surgery of the day
If you have diabetes and are about to undergo surgery, you will want to make sure to meet with your surgeon at least two weeks before the surgery to obtain orders for needed lab work. You will also want to discuss what to expect before, during, and after your surgery with your surgeon.
Make sure that during this appointment, you request that your surgery be one of the first cases on the list for the day. You will be fasting after midnight, and you don’t want to have a blood sugar drop during your surgery. Having your surgery first thing in the morning will help to avoid a low blood glucose.
Make sure to also meet with your endocrinologist or primary care provider a few weeks before the surgery. Ask them to write a letter to the surgeon, explaining to them that you have Type 1 or Type 2 diabetes.
The endocrinologist or PCP can let the surgical team know what to do to take care of your diabetes during surgery. If you use an insulin pump, your provider can make recommendations related to the basal rate for the pump (basal rates are often reduced to 80 percent during surgery).
The endocrinologist or the PCP could also make a recommendation to the surgical team to check your blood glucose every hour during the surgery. They may also need to adjust your blood sugar by giving you an intravenous dextrose drip.
Using an insulin pump during surgery
If you use an insulin pump, it may be possible for you to wear it during your surgery. You can usually wear it during surgery if your procedure will not be too long. Your provider can make recommendations related to the basal rate for the pump (basal rates are often reduced to 80 percent during surgery). Check with your endocrinologist to determine how much to adjust your basal rate.
Additional reading:
- Diabetes Experts Share Ways To Lower Your A1C Levels
- Closed Loop Systems: Future Treatment for Diabetes?
- Dietitians Answer Questions About Energy Levels, Picky Eaters, Plant Based Diet & More For Those With Type 2 And Prediabetes
- Can Diabetes Bankrupt a Country?
- Inside the Mind of Someone with Diabetes: Diana Vestal
It is also important to run your blood sugars a little bit higher than normal to avoid a low during surgery. One of my patients kept her blood sugar at about 135 mg/dl on the night before and the day of surgery. This allowed her to maintain blood sugars around 120 during her procedure. Conversely, the doctor will not want you to have a blood sugar that is excessively high.
Tips for recovery from surgery
As mentioned earlier in this article, stress causes elevated blood glucose. Pain is a stress on the body. Therefore, pain must be managed during surgery to combat stress hormones that are released when the body is in pain. These hormones elevate blood glucose. You may want to opt for a nerve block for anesthesia during surgery, due to it can keep you pain free for up to 12 hours after the procedure.
CGM and pain medications with acetaminophen
If wearing a Dexcom Continuous Glucose Monitor, you will want to ask the surgeon to prescribe pain medication without acetaminophen in it. This medication interferes with the sensor for these monitors. Oxycodone with ibuprofen would be a good option to avoid this problem.
Post-surgery SMBG
You will need to monitor your blood sugars often following surgery. The combination of stress hormones, pain, decreased activity, and decreased appetite, may make your blood sugars different than before surgery. With an insulin pump, your basal and bolus rates could also be different. One patient increased her basal rate of insulin, and used a conservative bolus. This ended up working out very well for her.8
Over to you
Have you been in a situation where you have had to take oxycodone or another form of opioid for pain management? How did it affect your diabetes? Did you get a high blood glucose? Did you get a low blood glucose? Were you hospitalized?
We would like to hear from you related to your experience of taking oxycodone or other opioids for pain when you have diabetes. Please let us know your thoughts in the comments section below.
Here at thediabetescouncil.com, we strive to provide you with the most comprehensive and up-to-date information to help you with your journey. Please let us know if you have enjoyed the article, if we left anything out, or just hop on the comment thread to say hello. Remember that we are here for YOU.
TheDiabetesCouncil Article | Reviewed by Dr. Sergii Vasyliuk MD on June 04, 2020
References
- http://www.netdoctor.co.uk/medicines/aches-and-pains/a27037/oxycodone-hydrochloride-uses-and-warnings/
- http://www.everydayhealth.com/drugs/oxycodone
- https://www.drugs.com/cdi/aspirin-oxycodone.html
- http://www.ncbi.nlm.nih.gov/pubmed/14499422
- http://www.medpagetoday.com/endocrinology/generalendocrinology/49006
- http://www.ehealthme.com/ds/oxycodone/high%20blood%20sugar/
- https://paindoctor.com/effects-opioids-diabetes/
- https://asweetlife.org/diabetes-and-surgery/